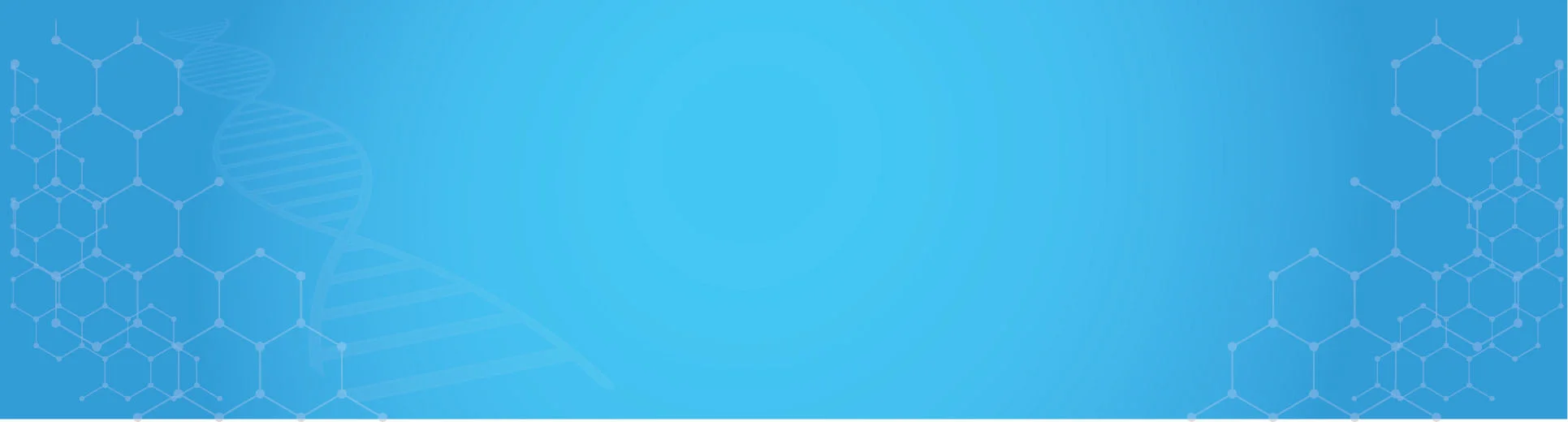
Rising Prescription Drug Costs
The escalating costs associated with prescription drugs are a primary driver in the Pharmacy Benefit Management Services Market. As healthcare expenditures continue to rise, employers and insurers are increasingly seeking effective management solutions to control these costs. Reports indicate that prescription drug spending has been growing at an annual rate of approximately 5 to 7%, prompting organizations to turn to pharmacy benefit managers for cost-effective strategies. These managers negotiate prices, implement formulary management, and promote the use of generics, which can lead to substantial savings. Consequently, the demand for Pharmacy Benefit Management Services Market is likely to increase as stakeholders aim to mitigate the financial burden of rising drug prices.
Growing Demand for Specialty Drugs
The increasing prevalence of chronic diseases and complex health conditions is driving the demand for specialty drugs within the Pharmacy Benefit Management Services Market. Specialty medications, which often require special handling and monitoring, are becoming a larger portion of overall drug spending. Reports suggest that specialty drugs account for nearly 50% of total drug expenditures, highlighting the need for effective management strategies. Pharmacy benefit managers play a crucial role in managing these high-cost therapies by implementing utilization management techniques and patient support programs. As the market for specialty drugs continues to expand, the demand for Pharmacy Benefit Management Services Market is expected to rise, as stakeholders seek to optimize the management of these complex therapies.
Increased Focus on Preventive Care
The shift towards preventive care is reshaping the Pharmacy Benefit Management Services Market. As healthcare systems emphasize the importance of preventive measures, pharmacy benefit managers are adapting their services to promote medication adherence and disease management programs. This trend is evidenced by the growing number of health plans that include preventive medications without cost-sharing, which encourages patients to utilize necessary prescriptions. By focusing on preventive care, pharmacy benefit managers can help reduce overall healthcare costs and improve patient outcomes. This evolving landscape suggests that the demand for Pharmacy Benefit Management Services Market will continue to grow as stakeholders recognize the value of preventive strategies in managing health.
Technological Advancements in Healthcare
Technological advancements are significantly influencing the Pharmacy Benefit Management Services Market. The integration of data analytics, artificial intelligence, and telehealth solutions is transforming how pharmacy benefit managers operate. These technologies enable more efficient claims processing, personalized medication management, and enhanced patient engagement. For instance, predictive analytics can identify patients at risk of non-adherence, allowing for targeted interventions. As technology continues to evolve, pharmacy benefit managers are likely to leverage these tools to optimize their services and improve patient care. This trend indicates a robust growth trajectory for the Pharmacy Benefit Management Services Market as organizations seek to harness technology for better outcomes.
Regulatory Changes and Compliance Requirements
Regulatory changes are a critical driver in the Pharmacy Benefit Management Services Market. As governments and regulatory bodies implement new policies aimed at improving healthcare access and affordability, pharmacy benefit managers must adapt to these evolving requirements. Compliance with regulations such as the Affordable Care Act and various state-level mandates necessitates that pharmacy benefit managers enhance their service offerings. This includes ensuring transparency in pricing and formulary management, which can lead to increased operational costs. However, the need for compliance also presents opportunities for growth, as organizations seek pharmacy benefit managers who can navigate these complexities effectively. Thus, the regulatory landscape is likely to shape the future of the Pharmacy Benefit Management Services Market.