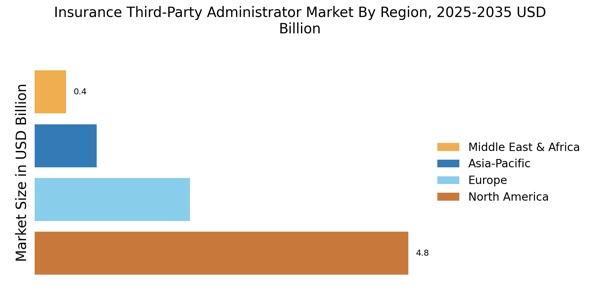
Rising Demand for Cost Efficiency
The Insurance Third-Party Administrator Market is experiencing a notable increase in demand for cost efficiency among insurers and policyholders. As companies seek to optimize their operational expenditures, the role of third-party administrators becomes crucial. By outsourcing claims processing and administrative functions, insurers can significantly reduce overhead costs. According to recent data, the market for third-party administration services is projected to grow at a compound annual growth rate of approximately 7% over the next five years. This trend indicates that insurers are increasingly recognizing the financial benefits of leveraging specialized administrators to enhance their service delivery while maintaining competitive pricing.
Growing Importance of Data Analytics
Data analytics is becoming increasingly vital in the Insurance Third-Party Administrator Market. Insurers are recognizing the value of data-driven insights to enhance decision-making processes and improve operational efficiency. Third-party administrators are leveraging advanced analytics to identify trends, assess risks, and optimize claims management. This trend is supported by findings that suggest organizations utilizing data analytics can improve their operational performance by up to 25%. As the insurance landscape becomes more competitive, the ability to harness data effectively will likely drive demand for third-party administrators who can provide these analytical capabilities.
Increased Focus on Customer Experience
In the Insurance Third-Party Administrator Market, there is a growing emphasis on enhancing customer experience. Insurers are increasingly aware that customer satisfaction directly impacts retention and acquisition rates. Third-party administrators are pivotal in this regard, as they streamline claims processing and improve communication channels. Data suggests that companies that prioritize customer experience can achieve up to a 20% increase in customer loyalty. As a result, insurers are investing in partnerships with third-party administrators that offer innovative solutions to enhance the overall customer journey, thereby driving growth in the market.
Regulatory Changes and Compliance Requirements
The Insurance Third-Party Administrator Market is significantly influenced by evolving regulatory changes and compliance requirements. Insurers are under constant pressure to adhere to stringent regulations, which necessitates the expertise of third-party administrators. These administrators help insurers navigate complex regulatory landscapes, ensuring compliance while minimizing risks. Recent data indicates that non-compliance can result in penalties exceeding millions of dollars, making the role of third-party administrators even more critical. As regulations continue to evolve, the demand for specialized compliance services within the third-party administration sector is expected to increase, driving market expansion.
Technological Advancements in Claims Processing
Technological advancements are reshaping the Insurance Third-Party Administrator Market, particularly in claims processing. The integration of artificial intelligence and machine learning is enabling administrators to process claims more efficiently and accurately. This shift not only reduces processing times but also minimizes errors, leading to improved customer satisfaction. Recent statistics indicate that the adoption of technology in claims management can reduce operational costs by up to 30%. As insurers increasingly seek to leverage these technologies, the demand for technologically adept third-party administrators is likely to rise, further propelling market growth.