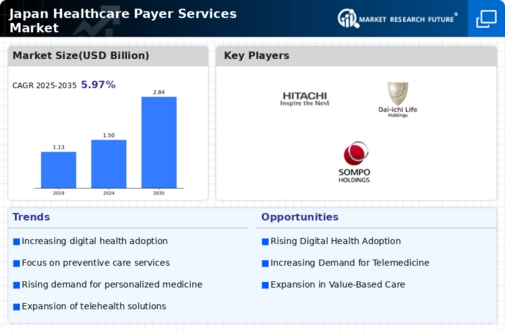
Focus on Preventive Care
The healthcare payer-services market is undergoing a paradigm shift towards preventive care, which is becoming increasingly prioritized in Japan. This focus is largely driven by the recognition that preventive measures can significantly reduce long-term healthcare costs. Payers are now incentivizing preventive services, such as regular health screenings and wellness programs, to mitigate the financial burden of chronic diseases. It is estimated that for every ¥1 invested in preventive care, there is a potential return of ¥3 in reduced healthcare costs. This strategic shift not only enhances patient health outcomes but also positions payers to better manage their financial risks. As a result, the emphasis on preventive care is likely to continue shaping the landscape of the healthcare payer-services market.
Increased Regulatory Scrutiny
The healthcare payer-services market is currently navigating an environment of increased regulatory scrutiny in Japan. Regulatory bodies are implementing stricter compliance measures to ensure transparency and accountability among payers. This trend is evident in the recent updates to the Health Insurance Act, which mandates more rigorous reporting and auditing processes. As a result, payer organizations are investing in compliance technologies and training programs to meet these new requirements. This heightened focus on regulation not only aims to protect consumers but also fosters a more competitive landscape among payers. Consequently, the healthcare payer-services market is likely to see a surge in demand for compliance-related services and solutions, as organizations strive to adhere to evolving regulations.
Rising Healthcare Expenditure
Japan's healthcare payer-services market is significantly influenced by the rising healthcare expenditure, which has been steadily increasing over the years. As of 2025, healthcare spending in Japan is estimated to reach approximately ¥42 trillion, reflecting a growth rate of around 4% annually. This increase is driven by factors such as the need for advanced medical technologies, higher costs of pharmaceuticals, and the demand for improved healthcare services. Consequently, healthcare payers are compelled to adapt their strategies to manage these rising costs effectively. This trend indicates a growing opportunity for payer-services providers to innovate and offer cost-effective solutions that align with the evolving needs of healthcare consumers, thereby fostering growth in the healthcare payer-services market.
Shift Towards Value-Based Care
The healthcare payer-services market is increasingly shifting towards value-based care models, which emphasize patient outcomes over volume of services provided. In Japan, this transition is being driven by both payers and providers who recognize the need for sustainable healthcare solutions. Value-based care models encourage collaboration among stakeholders, leading to improved care coordination and reduced costs. It is projected that by 2026, value-based care initiatives could account for up to 40% of total healthcare spending in Japan. This shift not only aligns with the goals of enhancing patient satisfaction but also positions payers to better manage their financial risks. As such, the healthcare payer-services market is likely to evolve in response to this growing trend, fostering innovation and new service offerings.
Technological Advancements in Healthcare
The healthcare payer-services market is experiencing a notable transformation due to rapid technological advancements. Innovations such as artificial intelligence (AI), machine learning, and big data analytics are enhancing operational efficiencies and improving patient outcomes. In Japan, the integration of these technologies is projected to increase the efficiency of claims processing by up to 30%. Furthermore, the adoption of telemedicine and digital health solutions is reshaping service delivery, allowing payers to offer more personalized care. This shift not only enhances patient engagement but also reduces administrative costs, thereby driving growth in the healthcare payer-services market. As technology continues to evolve, it is likely that payer organizations will increasingly invest in these solutions to remain competitive and meet the demands of a tech-savvy population.














Leave a Comment